Breast Cancer and the Brain
POSTED: 10/21/2022

Breast Cancer and the Brain
Friday, October 21, 2022
In the spirit of breast cancer awareness month, please enjoy this overview of the neurological complications of breast cancer!
Intracranial tumors:
The most common brain tumor in the united states is a metastatic cancer accounting for more than half of diagnosed intracranial tumors. That is, most tumors found in the brain are actually a spread of another cancer found elsewhere in the body. Much like infection, cancer cells have the ability to invade the vascular system. In doing so, they can travel to a site distant from the parent tumor and establish a nest at various sites, such as the brain. This is referred to as a metastasis. Several cancers travel to the brain the three most common being melanoma, lung cancer, and breast cancer.
Metastases can be solitary, but more often than not, occur at multiple different portions of the brain. When metastases occur, the involved brain region can experience local changes. The presence of the metastasis can trigger an inflammatory response in the brain which results in swelling. If the swelling is profound, it can compress adjacent brain structures such as the ventricles (the fluid filled chambers) or arteries/veins of the brain. Seeing as most tumors tend to be highly vascularized, metastases in the brain often bleed.
Depending on the location of the metastasis and involved adjacent structures, various neurological symptoms can arise. These include but are not limited to headaches, visual changes, nausea/emesis, weakness, sensory changes, slurred speech, loss of coordination, falls, loss of language ability, behavioral changes, and seizures. Metastases are typically diagnosed based on imaging findings in a patient with a cancer known to travel to the brain. At times, a biopsy or sampling of the spinal fluid is used to further improve the diagnostic yield. The treatment of metastasis depends on the source of the cancer, stage of the cancer, and the patient’s clinical status. But generally speaking, in addition to treating the original cancer, surgical resection, stereotactic radiosurgery (SRS), or whole brain radiation (WBRT) can be used under guidance of an oncologist.
Paraneoplastic syndromes:
When the human body is infected with a virus, fungus, parasite, or bacterium, the immune system is activated to eradicate the infection. This is also true for cancer. The immune system, admittedly not very well at times, recognizes cancer cells as foreign and produces immune cells (soldiers) and antibodies (weapons) to attack and kill the cancer cells.
Unfortunately, the antibodies (weapons) produced by the immune system are not always specific only to the cancer cells. These antibodies can sometimes bind to targets on the surface of nerve cells or inside them causing nerve damage. This is referred to as a paraneoplastic syndrome. Depending on the cancer, specific set of symptoms develop, at least in classic presentations.
Neurologic paraneoplastic syndromes are rare occurring roughly 1 in every 300 cancers. Over the years, more and more antibodies resulting in paraneoplastic syndromes have been discovered and linked to specific types of cancer. This list continues to grow enhancing the physician’s diagnostic accuracy and enhancing patient care through early detection. Most of the time, the cancer is diagnosed first with the paraneoplastic syndrome ensuing thereafter. However, in rare instances, the paraneoplastic syndrome develops first with a cancer eventually found at a later time.
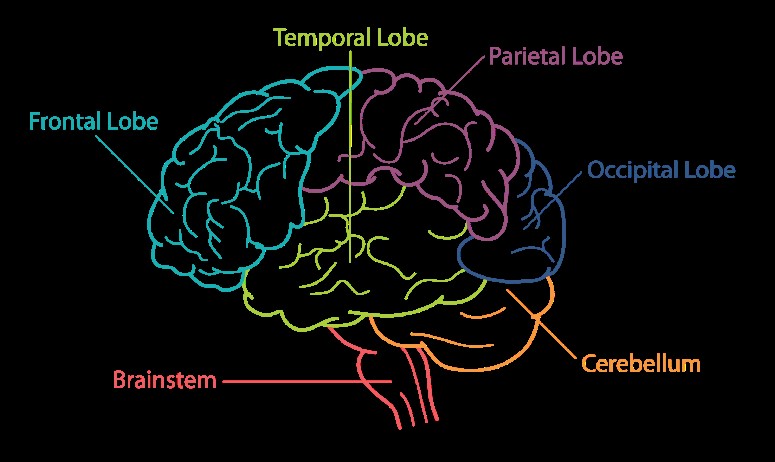
Paraeoplastic antibodies can bind any portion of the nervous system including the brain cortex (surface), brainstem (base of the brain), cerebellum (coordination center), spinal cord, nerve roots, peripheral nerve proteins, neuromuscular junction, and muscle cells. As such, the manifestation of paraneoplastic syndromes can be variable and includes headaches, seizures, memory loss, confusion, behavioral changes, involuntary movements, loss of coordination, vital signs abnormalities, weakness, incontinence, sensory changes, double vision, drooping eyelids, trouble swallowing, twitching, and pain.
Breast cancer is now recognized to result in several paraneoplastic syndromes through different antibodies with different binding targets. Below is a list of the common syndromes. Paraneoplastic syndromes are treated primarily by treating the underlying malignancy, at times employing immune suppressing therapies, and management of symptoms arising from the nerve damage.
- Stiff person syndrome (SPS): the target in this instance is the spinal cord through the Ampiphysin antibodies resulting in increased muscle tone/stiffness, trouble walking, and recurrent falls.
- Cerebellar degeneration syndrome: the target in this instance is a particular cell type referred to as Perkinje cells in the cerebellum through the antibody PCA-1/Yo. Since the cerebellum is heavily involved in coordination of motor function, patients often experience involuntary eye movements, loss of coordination, falls, slurred speech, and drunk like gait.
- Limbic encephalitis: the target in this instance is the limbic system of the brain through the antibody to AMPA receptors. The limbic system is the primitive function center. Patient typically experience seizures, memory loss, and psychiatric symptoms (anxiety, depression, hallucinations).
- Opsoclonus-myoclonus-ataxia syndrome (OMA): in this syndrome mediated through the ANNA-2/Ri antibodies, patient experience involuntary muscle twitching, involuntary eye movements, and loss of coordination.
Treatment related neurotoxicity:
While breast cancer does not directly result in the following neurological manifestations, the treatment of breast cancer, much like the treatment of various other malignancies, can. Two commonly employed modalities in treating cancer are chemotherapy and radiation. Both of those modalities can have toxic effects on the brain, spine, and peripheral nerves. Again, based on what is involved, the symptoms can be variable. Neurotoxicity can be reversible in certain instances but not always.
- Peripheral neuropathy: the chemicals used to kill cancer cells can be equally toxic to the body’s native cells including the nerves. One of the common side effects of chemotherapy used to treat various cancers including breast cancer is neuropathy. Neuropathy is a dysfunction of the peripheral nerves that can manifest as numbness, tingling, burning pain, sensitivity to touch, sensitivity to certain temperatures, and swelling. The neuropathy starts in the distal most end of the nerves (i.e the toes) and works its way back. The peripheral neuropathy of chemotherapy is a dose dependent process. That is, the longer the exposure and the higher the dose, the more likely an irreversible neuropathy occurs. Common neuropathy causing agents include Platinum drugs (Cisplatin, Oxaliplatin), Taxanes (Paclitaxel), and Vinca alkaloids (Vincristine, Vinblastine).
- Encephalopathy: this is a nonspecific term signifying brain dysfunction. It often presents as confusion and disorientation of the patient closely related to an exposure. This is typically reversible after the exposure has been discontinued. This can be seen with both radiation and chemotherapy.
- Posterior Reversible Encephalopathy Syndrome (PRES): this entity is most often seen with poorly controlled hypertension. However, with certain cancer treatments, PRES can occur. Simply put, the arteries of the brain become leaky resulting in brain swelling. The swelling most commonly occurs in the posterior head region, but can take place in any location of the brain. Symptoms include confusion, seizures, headache, vision changes, weakness, and sensory changes.
Dr. Oliver Achi, Neurologist, Medical Director of Neurology Services, Iberia Medical Center
Appointments with Dr. Achi: 337.374.7242
