Stroke Awareness: Hemorrhagic Stroke
POSTED: 5/11/2022

Stroke Awareness: Hemorrhagic Stroke
Not All Strokes are Created Equal
What is hemorrhagic stroke?
Strokes are sudden and catastrophic brain attacks that can result in long lasting disability. And while the majority are ischemic, hemorrhagic events can account for up to 13% of strokes and will be the focus of this overview. Hemorrhagic stroke in most of its forms can be severely disabling with a negative impact on a patient’s quality of life much like ischemic stroke. Before we delve into the different types of hemorrhagic strokes, a brief review of the anatomy of the brain might be useful.
Where is the blood going?
The brain is separated from the skull by three layers of tissue collectively referred to as the meninges. The first layer, the pia mater, directly lines and adheres to the surface of the brain. The second layer, the arachnoid mater, is separated from the pia mater by the arachnoid space which houses arteries and veins of the brain (among other vital structures). And finally, the third layer, the dura mater (or “tough mother”), a band of dense connective tissue tops the arachnoid matter. Hemorrhagic strokes can arise in the brain or in these various compartments as discussed below.
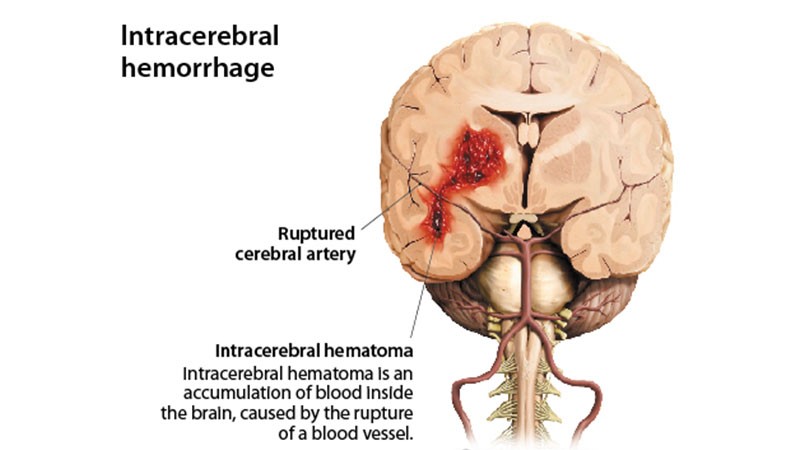
What is an intracerebral hemorrhage?
A hemorrhage within the brain itself is called an intracerebral (ICH). When you think of ICH, think of uncontrolled high blood pressure as it is the most common cause. Other causes include but are not limited to use of blood thinners, use of recreational stimulants, various bleeding disorders, vascular malformations, blood clots in the veins of the brain (venous thrombosis), an ischemic stroke that then bleeds, brain tumor, inflammation of the brain arteries (vasculitis), and infections. Increasing the risk of an ICH are advancing age, heavy alcohol consumption, smoking, obesity, sedentary lifestyle, low LDL (bad cholesterol) levels, and ethnicity (with a higher prevalence in African American patients).
An ICH can be easily diagnosed with a CT scan and or brain MRI. Treatment of an ICH involves controlling the blood pressure, relieving build up of pressure in the brain through shunt devices, and when necessary removing portions of the skull and evacuating the blood collection. The ultimate treatment however is reducing modifiable risk factors for ICH.
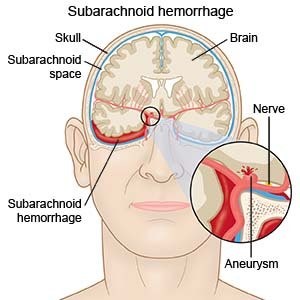
What is a subarachnoid hemorrhage?
A hemorrhage arising between the pia mater and arachnoid mater, or the subarachnoid space, is referred to as a subarachnoid hemorrhage (SAH). While a SAH can be traumatic in nature, meaning secondary to a traumatic brain injury, it can be spontaneous with the most common cause being a ruptured aneurysm (85% of cases of spontaneous bleeds).
An aneurysm is an outpouching or balloon like dilation of an artery that can rupture resulting in 51% fatality rate and significant disability in half of survivors. Aneurysms can be present at birth or develop later in life as a consequence of high blood pressure and smoking among other predisposing factors. This type of stroke requires immediate medical attention or otherwise very poor outcomes are likely.
Risk factors for rupture of a preexisting aneurysm include high blood pressure, smoking, larger size, location, shape, advancing age, female gender, and ethnic background (with higher incidence in African American, Hispanic, Japanese, and Finnish patients). Treatment of a ruptured aneurysm involves controlling blood pressure and surgically securing the aneurysm by deploying a clip across its neck or a coil within the aneurysm body itself.
Other causes of spontaneous SAH include but are not limited to a tear in the wall of an artery (arterial dissection), venous bleeding (perimesencephalic SAH), vascular malformations, bleeding disorders, stimulant use, vasculitis, and venous thrombosis. SAH can be diagnosed via head CT and or brain MRI and aneurysms are diagnosed using angiography (pictures of the arterial tree of the brain). Seldom, imaging may not demonstrate the blood or the aneurysm in which case physicians may rely on additional testing such as lumbar puncture (spinal tap) and advanced spinal imaging.
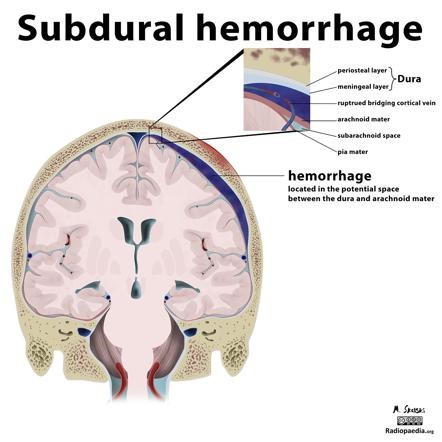
What is a subdural hemorrhage?
A hemorrhage arising between the dura mater and arachnoid matter is referred to as a subdural hemorrhage (SDH). And while this type of stroke can be just as disabling as ischemic strokes, ICH, and SAH, more often than not, patients tend to have better outcomes, specifically depending on the underlying cause. The incidence of SDH hemorrhage increases with increasing age.
Head trauma (motor vehicle accidents, fall, and assault) is the most common cause of a SDH by way of injuring veins (bridging veins) of the brain. Other causes include and are not limited to low intracranial pressure, a ruptured aneurysm, vascular malformation, tumor/cancer, inflammatory conditions, infections, blood thinner use, and bleeding disorders.
A SDH is easily diagnosed with a head CT and or brain MRI. Treatment of a SDH depends on the size of the bleed, its regional effects on adjacent brain, active bleeding, and the patient’s mental status. While often observation and discontinuing blood thinning medications is sufficient, surgical intervention and reversal of a bleeding disorder may sometimes be necessary. The two main surgical techniques involve placing a drain in the area of hemorrhage to alleviate the build-up of blood and or removal of the skull temporarily to evacuate the collection of blood.
What happens during a hemorrhagic stroke?
Much like in ischemic stroke, hemorrhagic stroke can result in a focal neurological deficit. This includes but not limited to one sided weakness/numbness, facial droop/facial numbness, slurred speech, trouble swallowing, trouble speaking, trouble understanding, vision loss, double vision, partial visual field loss, and vertigo.
However, in addition to the above, hemorrhagic strokes can often result in sudden and severe headaches which are usually out of character and should always prompt immediate medical evaluation. In addition, hemorrhage in the brain can result in sudden increase of pressure which may result in loss of consciousness, nausea, vomiting, somnolence, and even coma. Lastly, through irritating the covering of the brain (meninges discussed above) patients may experience neck stiffness and sensitivity to light.
In other words, if you suddenly experience the worst headache of your life that is new and unlike prior headaches, or if you experience any of the other symptoms discussed, please go to the emergency room immediately for evaluation.
Have you been taking care of your brain health?
As you may have already noticed, several risk factors seem to be at play among ischemic as well as different types of hemorrhagic strokes. Thankfully, some are modifiable and in your control. Healthy living which includes controlling some of these risk factors can substantially reduce your risk of stroke overall. Below is a list of things that can go a long way in protecting you.
- Consider checking your blood pressure once weekly and if it is persistently elevated above 130/90, speak to your primary care physician about lifestyle modification, dietary choices, and medications.
- Have routine wellness visits with your primary care physician where they will check you for diabetes and cholesterol disorders and treat them accordingly.
- Lead an active lifestyle and attempt aerobic exercise at least three times weekly for 30 minutes at a moderate intensity. This can be brisk walking, biking, running, and or swimming.
- In addition to the risk of lung cancer, smoking can substantially increase the risk of an adverse cardiovascular event such as stroke or heart attack. If you are interested in quitting (which is highly recommended), speak to your primary care physician about smoking cessation programs, aids, and medications.
- Minimize your alcohol intake. Moderate to heavy consumption of alcohol is considered two or more drinks daily for men and one or more drink daily for women. If interested in quitting, please talk to your provider.
- If you know of any family members who have been diagnosed with an aneurysm, specially a ruptured aneurysm, or vascular malformation, speak to your physician about screening.
- Make sure you tell your doctor about all medications you take, including supplements, over the counter medicines, and herbal remedies as a lot of them can have blood thinning properties.
- If your family has a known history of blood clotting or bleeding disorders, make sure you inform your physician to include this information in your medical record. This should include miscarriages, personal or in the family.
- If your weight is more than desired for your height (which can be simply determined at your next office visit) speak to your doctor about weight loss. Even a small amount of weight loss can substantially reduce your blood pressure, improve your diabetes, and subsequently your overall health and longevity.
- If you snore, stop breathing in your sleep, or often feel the need to nap in the daytime, talk to your doctor about your symptoms. You may have sleep apnea which is a recognized risk factor for ischemic strokes.
- Refrain from using recreational drugs, especially stimulants such as cocaine, amphetamine, methamphetamine, ecstasy, bath salts, and Kush. These drugs can dangerously elevate blood pressure and result in arterial spasms that can subsequently lead to ischemic stroke, hemorrhagic stroke, and or heart attacks.
Dr. Oliver Achi, Neurologist, practices at Iberia Medical Center. His office is located at 2312 East Main Street, Suite C, across from the IMC Main Campus. For appointments or more information, call 337.374.7242.
